
Whether you’re a family member to someone with diabetes or are a direct care worker, being a caregiver for a diabetic patient can get overwhelming fast. You may be juggling multiple visits to specialists, constantly taking inventory and restocking a long list of diabetes care supplies, checking lab work results online, or trying to follow their doctor’s insulin therapy protocol.
You may have many questions. Can they eat that piece of pie? What do you do when they feel dizzy?
In this post, we’re stepping you through some of those questions – showing you how to care for a diabetic senior well and what you can expect along the way. I also share my personal experiences, as a caregiver to a child with type 1 diabetes and someone with both grandparents and in-laws who have type 2 diabetes.
Table of Contents
- Type 1 vs Type 2 Diabetes
- The Challenges of Caring for an Elderly Diabetic Patient
- Comorbidities and the Cocktail of Medications
- Blood Sugar Levels
- Recognizing an Emergency for Diabetic Seniors
- Long-Term Risks of Poorly Controlled Diabetes in Older Adults
- Caregiver Tools and Resources to Manage Diabetes in Seniors
- The Diabetes Care Team
- Keeping Inventory of Diabetes Supplies
- Finding Free and Low Cost Medication and Supplies
- Dialysis
- Conclusion
Type 1 Diabetes vs Type 2 Diabetes

To begin with, we need to distinguish between type 1 and type 2 diabetes. While the conditions are similar and are often confused, there are notable differences. To provide the best support for your family member, you need to know the type they have and how to treat it.
Type 2 Diabetes
Type 2 diabetes accounts for between 90% and 95% of all diabetes and in the United States it is the 7th leading cause of death. As such, if you’re a caregiver for a diabetic patient, you’re probably supporting someone with type 2 diabetes.
Type 2 diabetes is strongly associated with lifestyle factors, including obesity and low physical activity. Having a family history of diabetes or being more than 45 years of age can also increase your risk.
The prevalence of type 2 diabetes is even higher among racial/ethnic minority groups. A study of older Medicare members shows the prevalence of type 2 diabetes to be particularly high for African American (37%) and Hispanic/Latinos (38%). They are also more likely to be diagnosed at a younger age.
With almost one in four seniors aged 65 and older estimated to have type 2 diabetes, caring for an older family member or client with the condition is becoming all too common. Doing so requires special attention of caregivers and a basic understanding of the condition’s usual ailments and approaches to helping them stay in control of their diabetes care regimen.
Type 1 Diabetes
Type 1 diabetes, on the other hand, is an auto-immune disorder. Research suggests that viral infections can trigger the body’s auto-immune system to attack the pancreas, preventing it from creating enough insulin. A family history also increases the risk of developing type 1 diabetes.
Type 1 diabetes used to be known as juvenile diabetes; however, about 40% of patients are diagnosed at the age of 30 or older. Persons with type 1 diabetes are living with the condition longer than ever before and entering old age. Lifestyle factors have nothing to do with one’s risk. A person with type 1 diabetes did not ‘get’ diabetes from overeating or having too many sweets.
With type 2 diabetes, weight loss and a strict diet may allow people to avoid diabetes medications for some time. This isn’t the case with type 1 diabetes.
You should also know that people with type 1 diabetes are often offended at suggestions from others that a dietary change alone will help them treat their diabetes.
Unlike with type 2 diabetes where insulin is only needed in the most severe cases, people with type 1 diabetes cannot make their own insulin and they require daily insulin right out of the gate from diagnosis.
To date, no prescription or diet alone can help manage type 1 diabetes.
Also be aware that some people with type 1 diabetes are misdiagnosed as having type 2. If your family member was diagnosed as having type 2 diabetes and isn’t responding well to treatment, it may be worth getting them tested to find out whether they actually have type 1 diabetes.
Symptoms of Diabetes
Many people aren’t aware that they’re living with diabetes, so it’s important to be aware of the symptoms common to both types, including the following.
- Frequent urination
- Increased thirst
- Weakness and fatigue
- Blurry vision
- Slow healing of cuts and bruises
- Mood changes or irritability
- Unintended weight loss (type 1)
- Numbness, tingling, or pain in hands and feet (type 2)
The Challenges of Being a Caregiver for a Diabetic Patient
Caregiving for a diabetic senior is more complicated than supporting a non-diabetic in a variety of ways. Because of this, the caregiver needs to be aware of the challenges and know how to meet them. The caregiver may be heavily involved in continuous health monitoring and implementing the diabetic seniors’ prescribed treatment, especially if the senior struggles to do so themselves.
In this section, we’re highlighting the key areas that you need to be aware of and how you can best protect the senior’s health.
Remember too that some approaches will vary depending on whether the senior has type 1 or type 2 diabetes.
Understand the Disease and Warning Signs
Professional caregivers should be well-informed about diabetes, symptoms, and emergencies that can occur. If recently diagnosed with the disease, the family members may take some time to learn the ins and outs. You must know things such as:
- The A1c levels of the senior
- The senior’s other health conditions (or ‘comorbidities’)
- Symptoms and known complications
- Prescribed medications
- Insulin protocols
- Schedule for routine check-ins with the primary care provider and/or specialists
Medication Regimen
Adhering to the senior’s medical care treatment is the cornerstone of optimal diabetes care management. Caregivers should strictly follow the doctor’s instructions.
Insulin Protocol
Insulin therapy is the primary treatment approach for patients with type 1 diabetes and is sometimes used for type 2 diabetes, if the patient is unable to keep their blood sugar levels within a healthy range.
The doctor may recommend various forms of insulin therapy based on the patient’s hemoglobin A1c levels, their weight, and insulin resistance, as well as the results of other blood work such as lipids and vitals, like blood pressure.
Many seniors who were diagnosed with type 1 diabetes at a younger age may have grown accustomed to using needles to inject their insulin. However, an increasing number are opting for the latest technology to help them administer insulin and regulate their blood glucose using insulin pumps and monitoring their glucose with Continuous Glucose Monitors (CGMs). Each approach has its pros and cons, and nuances that you’ll need to explore with the senior to determine their comfort level.
The caregiver and family members must understand the appropriate protocol and follow the instructions of the physician.
Typically, diabetes health educators at the diabetic’s primary care doctor’s office or endocrinologist can recommend dietary changes. Never hesitate to ask them questions or set up a time to meet to discuss any reservations you have or confusion about what everything means.
Adopting a New Diet and Lifestyle
Diet is one of the primary ways that providers encourage anyone with diabetes to keep their glucose levels in a healthy range. Healthy food choices can help to keep the blood glucose level within the target range.
Reluctance to switching to healthier alternatives is an expected reaction in many diabetic patients.
Family members can motivate diabetic seniors to adopt dietary changes slowly, making incremental changes. One way to show support for the diabetic senior is to get the whole family on board with the same dietary changes and new menus.
Finding delicious diabetic friendly meals can help as well, like these 13 Mexican-inspired diabetic meals for seniors.
For individuals with type 1 diabetes, attention to diet takes on a very different meaning. Low carb diets can go a long way to reducing the number of sugar spikes and lows they experience throughout the day, any and all carbs need to be chased with some amount of insulin.
The senior’s endocrinologist or diabetes educator will instruct the caregiver on the proper carb ratios to use with the senior’s insulin pump or through administration via needle or pen. These ratios will help you calculate how much insulin to administer to account for the amount of carbs consumed. Every single morsel of food requires insulin; and hence, proper planning.
For both types of diabetes, you’ll quickly become accustomed to spotting which carbohydrates tend to spike their blood glucose. Fruit like watermelon and bananas might be the culprit for some individuals; for others, even alleged ‘sugar free’ foods or products with sugar substitutes may spike their sugar.
Many people with type 1 diabetes will report that meals like pizza will keep their blood glucose levels high for a sustained period.
Periodic Health Monitoring and A1c Testing
Regular health checkups, including regular A1c testing with a lab is part of the diabetes management program, making them highly relevant to any caregiver for a diabetic patient too. Visit the doctor at the scheduled time, take note of the glucose readings, and follow other instructions.
An A1c test captures the patient’s blood glucose levels in the past 3 months. If their A1c levels are on the high end, the senior’s medical provider may recommend testing every 4 months (or 4 times per year). Get comfortable with your local laboratory, their schedules, and the best time to come in for testing.
Caregivers should also monitor the senior closely to see how well they respond to the treatment.
Comorbidities and the Cocktail of Medications

The term comorbidities refers to slew of other health conditions that accompany type 2 diabetes and may or may not relate to diabetes directly, such as asthma. Some of these conditions may have been present before diabetes diagnosis, while others may develop after. For example
- Arthritis may have developed after the diabetes diagnosis, but is not presumed to be directly connected.
- Partial blindness can occur as a result of diabetes, but it may also have arisen due to other childhood conditions.
According to the American Diabetes Association (ADA), about 40% of adult diabetic patients have at least 3 or more comorbidities. Multimorbidity is a common occurrence in senior diabetics. Seniors with diabetes may have some common comorbidities such as hypertension, overweight/obesity, cardiovascular diseases, kidney complications, and other conditions.
Dealing with comorbidities is the toughest challenge for health care providers and family members. They must address these conditions alongside diabetes care, oftentimes juggling multiple medications and therapies for each.
Indeed, more than a third of the prescription medications taken each year are for seniors, with many filling between 9 and 13 prescriptions each year.
Medications and Care Coordination
Addressing comorbidities with diabetes through comprehensive treatment and home care is critical to preventing coma and other life-threatening conditions. Special attention should be paid to the interaction between medications taken for each condition and to any new symptoms or side effects.
While coordination of care between providers is always the goal, our health care system is very complex. If you’re filling prescriptions at the same pharmacy (always recommended), ask to speak to the pharmacist to verify any potential interactions between newly prescribed medications.
Never, EVER assume that there is any communication between the senior’s primary care provider and the various specialists.
Too often, seniors are prescribed medication by a new specialist (be it, a nephrologist, neurologist, or other) or by an emergency care provider following a hospitalization. Yet, no one ever stops to consider how the medications interact with each other.
Sometimes, the senior may even end up with multiple prescriptions for medications intended to treat the same condition. Can you imagine the outcome if a senior is prescribed two different medications, both used for reducing blood pressure? It’s enough to require a prescription for anxiety.
There are other complications with medications too, including:
- The fact that a new doctor may not know why some medications were prescribed, particularly if they were prescribed for an off-label use. They may choose to continue those medications, despite not knowing, which can lead to the senior taking medication that is no longer needed.
- Medication cascades, where patients are taking one medication to mitigate the side effects of another medication, then a new one to mitigate new side effects. These cascades can be avoided by choosing the initial medications better or by making lifestyle changes rather than relying on medication.
- Forgetting medications or taking more than is needed. The more medications a senior is taking, the easier it is to lose track. For some medications, the consequences of skipping a dose or double dosing are minor. Other times, the consequences can be severe and even send the senior to the hospital.
- Medications can also interact with some foods and supplements.
These issues mean that it’s always important to enquire about medications and pay close attention to side effects. Try to find out what the purpose of each medication does, along with whether it is truly needed. Asking these questions can help to refine the senior’s medications and create a safer balance.
Diabetes Help? For more tools to help track your diabetes supplies, learn more about our tracking sheet.

Mental Health Impacts
There’s also the mental health aspect of diabetes care to talk about.
Stress, anxiety, and frustration are common in seniors. The onset of a new disability, and the limitations it brings with it, may be disconcerting for many. The condition can become worse due to changes in diet, lifestyle, and intensive medical treatments, such as dialysis or vision impairment.
Seniors will require a lot of love, care, attention, and moral support from caregivers and family members in accepting these changes.
Joining a diabetes support group can be beneficial for you and the senior. Support groups help to decrease isolation, giving people the sense that others are in the same boat.
The American Diabetes Association (ADA) is also tapped into Aunt Bertha’s extensive repository of community resources that you can search through for just about anything, from help with transportation to accessing disability benefits and more.

Diabetes and Depression
Even more concerning is the intersection between diabetes and depression. In particular, having diabetes increases your depression, while being depressed increases your risk of type 2 diabetes and can make diabetes management more difficult.
After all, people who are depressed often struggle with even the basic tasks of life, including staying clean, eating good food (sometimes eating anything is an immense challenge), and even getting out of bed. Trying to follow a diabetes regimen when depressed may feel impossible.
Thankfully, diabetes and depression can be treated together and some treatment approaches, like exercise and weight loss, can help both conditions at the same time.
If the senior is showing any symptoms of depression, including being overly pessimistic, it’s important to talk to their doctor about depression and treatment approaches. This way, the treatment and advice can be tailored to meet the senior’s current needs.
Mobility Issues
Physical disability and cognitive impairment are other known threats to the wellbeing of seniors with type 1 or type 2 diabetes, especially if the senior has had extended periods of poorly controlled diabetes. Studies have linked diabetes to increased likelihood of complications in neuropsychological functions, mobility syndromes, and partial or full disability.
A decline in cognition can make it more difficult for seniors to perform basic tasks, such as dressing themselves or walking independently.
Caregivers will need to be ready to accommodate the senior’s slow gait or have assistive devices on hand (which are described later). You may need to opt for a scooter or even a wheelchair for the senior at the grocery store or mall, or bring your own seating if you anticipate long wait lines.
COVID 19
Studies show that people with either type of diabetes are at greater risk of experiencing complications from COVID-19.
Not only did people with diabetes infected with COVID-19 fare worse in their recovery and mortality, but many scientists are also finding a strong link between COVID-19 infection and the onset of new type 2 diabetes. This means that we can fully expect a huge wave of new cases, as we unravel the true long-term impact of COVID-19.
Blood Sugar Levels
Blood glucose testing is a well-known part of diabetes management.
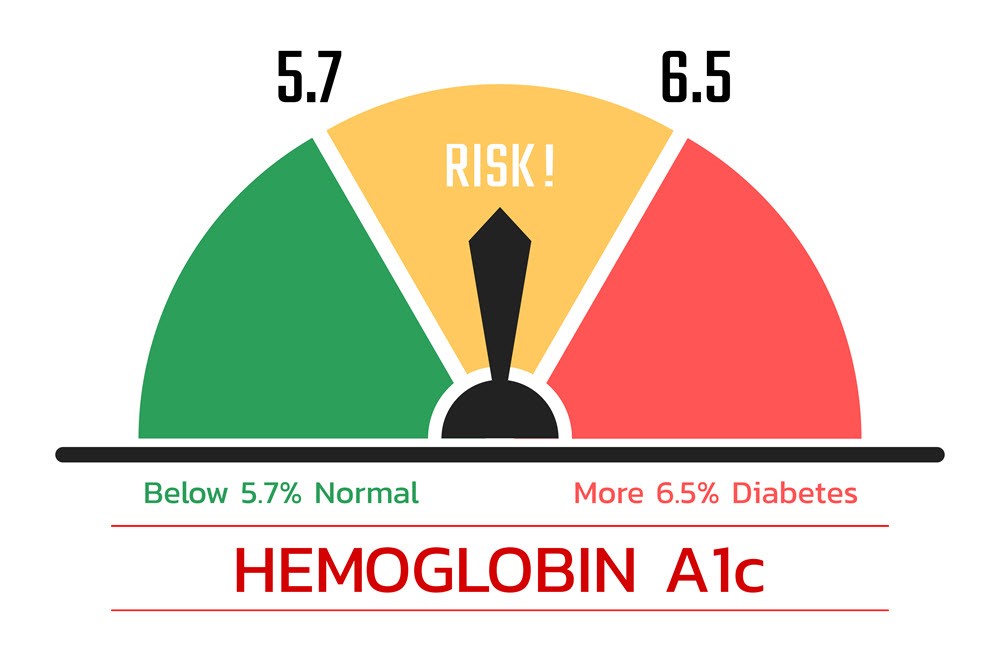
The doctor may refer the patient to a lab for an A1c test (hemoglobin A1c/HbA1c) as many as 4 times per year, prior to a routine check-up or based on any apparent symptoms. Some providers have on-site testing capabilities, referred to as ‘point of care’ testing. The test shows the average blood sugar level in the body over the past 3 months.
The readings from the A1c test reports clearly depict whether a person has prediabetes or diabetes. This is the first step in diabetes management. The A1c levels in the result help you determine what you need to do further.
The American Diabetes Association defines the levels like this, as do the NIDDK and CDC:
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or above
The guidelines are intended for the average adult. They can apply to older adults when they are otherwise healthy and functional, don’t have cognitive impairment, and are projected to have a decent life expectancy.
However, while most doctors aren’t calculating their patients’ life expectancy, they do recognize that A1c requirements may be relaxed for older adults who are dealing with multiple health conditions, such as hypertension (high blood pressure) and hyperlipidemia (high cholesterol).
Improvements in A1c levels may be more cause for celebration and a desired treatment goal than trying to get them to a specific range.
Still, minimizing hyperglycemia (high, sustained glucose levels) and the consequential complications is a goal common to all persons with diabetes, regardless of age.
How Often Should Levels Be Tested?
Once diagnosed with diabetes, the senior needs to have adequate diabetes management to keep the blood glucose levels within the normal range. The physician will determine the frequency at which the person may require a test, depending on the severity of the condition.
The senior may need to check the readings with a glucometer at home at least once a day or even more, especially before and after a meal. Nowadays, it is easy to do so with a Continuous Glucose Monitor (CGM) device to avoid pricking one’s fingers.
Recognizing an Emergency for Diabetic Seniors

Diabetic patients, especially older adults, need consistent caring and blood sugar monitoring. The family members or caregivers must keep a watch on the blood glucose readings and insulin therapy. If blood sugar level and insulin are out of balance, the patient may show signs of emergency (which may be life-threatening). At this point, the person may need someone’s help to overcome the crisis.
Here are the most important areas to watch out for.
Hypoglycemia
Hypoglycemia simply means low blood sugar levels in the body. The glucose level can drop in diabetic patients due to various reasons:
- Skipping meals
- Too much physical activity
- Insulin overdose or miscalculation
- Alcohol consumption
Patients generally recognize this condition from mild symptoms like shakiness or hunger. But in the case of acute conditions, they may suffer outcomes like diabetic coma, seizures, blurred vision, or fainting.
Diabetic Ketoacidosis (DKA)
Lack of sufficient insulin in the body prompts the liver to break fat into ketones rapidly to provide energy. The buildup of ketones in the bloodstream can be damaging throughout the body. This is a life-threatening condition where the individual can fall into a coma.
Hyperosmolar Hyperglycemic Syndrome (HHS)
This is a relatively rare phenomenon that can occur in patients with type 2 diabetes with very high blood glucose levels (600mg/dL) and low to no ketones. The condition is evident in seniors with uncontrolled diabetes alongside acute illness or infection. HHS can lead to seizures, coma, and even death.
Long-Term Risks of Poorly Controlled Diabetes in Older Adults
Why is your help as a caregiver so vital?
For one thing – poorly controlled hyperglycemia has been linked to multiple comorbidities in seniors. Long-term diabetes can damage the vital organs and even lead to some severe life-threatening illnesses.
Diabetics aged 75 years or higher are at a greater risk compared to those in the age group of 65 to 74 years. With aging, prolonged history of diabetes can cause both vascular and non-vascular complications including some of the following issues:
Peripheral Neuropathy (nerve damage)
A microvascular disease, neuropathy can be evident in the form of nerve pain, foot ulcers, loss of sensation, difficulty in balancing, etc.
Myocardial Infarction (heart attack)
Seniors with type 2 diabetes are at a higher risk of cardiovascular diseases especially myocardial infarction (MI).
It is one of the prime causes of mortality and morbidity in diabetic individuals.
Gradual increase in thrombosis and formation of atherosclerotic plaque can occur due to high blood sugar. The conditions can worsen due to delayed treatment and trigger the risk of heart attacks from MI.
Retinopathy
Elderly patients diagnosed with type 2diabetes between the ages of 40 and 64 years of age are at a greater risk of developing retinal diseases which may lead to loss of vision later in life.
Alzheimer’s Disease/ Vascular Dementia
Diabetes can lead to the development of vascular and non-vascular diseases in patients with type 2 diabetes. High blood sugar levels are associated with an increased risk of developing dementia in old age.
Diabetes can cause potential damage to the blood vessels. The reduction or blockage of blood flow to the brain is one of the major causes of vascular dementia. As a result, cognitive impairment or decline is evident in the form of memory loss, thinking inability, difficulty in concentrating, communication problems, etc.
Caregiver Tools and Resources to Manage Diabetes in Seniors
Diabetes management is made easier with many modern tools and technologies. From blood glucose monitoring to a healthy diet, a series of tools and resources can make the entire process less daunting.
1. Continuous Glucose Monitors (CGM)

Blood glucose meters (or glucometers) used to be the go-to for checking glucose levels throughout the day, requiring one to pierce their finger with a lancet. Luckily, new devices are abundant on the market thanks to companies like DexCom and Insulet. For persons opting to use continuous glucose monitors (CGMs), the glucometer is used as a backup or to validate or calibrate the CGM’s readings as recommended by the manufacturer.
A CGM device can be attached to the arm and provides a constant read on fluctuating blood glucose levels. Alarms can be programmed at various levels, such as to alert the user when their blood glucose is below 80 or when they are over 180 for an extended period of time.
You can see trends over the past hour, 3 hours, 6 hours, 12 hours, or 24 hours and note patterns. The graphs make it easy to anticipate when your glucose may dip below the desired level. Or conversely, notice when your glucose is rising beyond your range.
Caregivers can receive the glucose reading on their smartphone connected to the app that is paired to the CGM device. You can receive the signal at the grocery store or down the street and get an immediate alert if the senior in your care has a glucose level that is dropping fast.
The CGM companies provide a warranty and 24/7 customer service and technical support. Most caregivers involved with CGM’s typically have the company on speed dial.
2. Insulin Pens and Ultra-Fine Pen Needles

Every diabetic patient wishes to have pain-free insulin injections. The newest insulin pens have the option to be used with ultra-fine pen needles. The insulin pens come in 1 and ½ units. The needles have thin precision sharp tips to minimize the penetration force and discomfort.
3. Diabetes Management Apps
Nowadays caregivers use a series of diabetes management apps to track food calorie quality, carb counts, weight, and so on.
One innovative tool worth mentioning is Fooducate (available for Apple and Android). The app helps you count the carbohydrates and other nutrients in your food, or calculate your overall calorie consumption.
Medical ID is another essential tool for Android smartphone users. It offers medical information to deal with emergencies. Setting the patient’s profile helps the caregivers to store information such as allergies, medical contacts, available medicines, etc.
There are plenty of other apps for caregivers too, including ones for storing health information and communicating with other members of the care team. While these apps aren’t designed for diabetes specifically, they can still make your life much easier.
4. Instructional Videos
Caregiver resource sites, such as the Caregiver Action Network or AARP’s library of caregiving videos offer caregivers an array of tutorials on many subjects. There are several popular YouTube channels with videos for diabetic seniors.
The caregiver for a diabetic person can follow the exercises and tips to help the older adults with managing their diabetes, checking their feet, staying active, and preparing for a doctor’s appointment.
Here are some interesting videos to get you started:
Keep in mind that if you’re just learning how to use a new diabetes insulin pen, glucometer, or insulin pump, most manufacturers will have their own library of instructional videos to walk you through the steps.
5. Healthy Alternatives Cookbooks
Whether your loved one has a taste for Mexican or Soul Food, you can find healthy alternatives to these meals in many cookbooks. If you’re just getting started and maybe not the best cook, various cookbooks cater to your needs. Here are just a few.
We also have some delicious recipe roundups on our site:
6. Assistive Devices
We have a series of articles providing a more in-depth description of clothing, footwear, and devices that caregivers can use to make day-to-day care easier. These can make dressing, bathing, and eating more hassle free.
Adaptive clothing and footwear is particularly important for seniors with diabetic complications, like wounds or fluid retention. These complications can make regular clothing and footwear difficult and uncomfortable.
Take a look at some of the articles below for further information:
- Adaptive Footwear for Seniors to Make Mobility Easier
- Adaptive Caregiving Tools and Skills that are Worth Trying
- 7 of the Best Adaptive Shoes for Seniors
If you are worried about the costs, we have you covered. You can find tips for paying for assistive devices here.
7. Online Resources and Support Groups

American Diabetes Association (ADA)
Support groups help to decrease isolation, giving people the sense that others are in the same boat. The American Diabetes Association (ADA) are also tapped into Aunt Bertha’s extensive repository of community resources that you can search through for just about anything, from help with transportation to accessing disability benefits and more.
The Association of Diabetes Care and Education Specialists (ADCES)
The Association of Diabetes Care and Education Specialists (ADCES) has a database that you can search to find a free diabetes education program near you. These classes typically run for about 6 weeks, meeting once a week for two hours and providing invaluable information for caring for a loved one with type 2 diabetes.
JDRF (Juvenile Diabetes Research Foundation)
Despite its name, JDRF’s TypeOneNation Community Forum attracts mostly adults who have aged into adulthood or old age with type 1 diabetes or their family members. There is a dedicated, knowledgeable moderator. I have found the advice on here to be unparalleled.
You can also submit a question to their volunteers who can provide one-on-one support, although medical or legal advice isn’t offered.
Type 1 Reddit
Here’s a place to share your successes, vent, get tips, or check in with others on just about anything related to type 1 diabetes care. I’ve gotten great tips from other users here, such as how to travel and get through TSA with a bag of diabetes supplies.
The Diabetes Care Team
Being a caregiver for a diabetic patient doesn’t mean that you’re going it alone. Instead, there are other people involved in care as well and one of your key tasks will be coordinating between the various care providers. Our complex healthcare system, despite the medical advances, still lacks in its sophistication to share basic information between logical parties. That’s where you come in.
The patient. To the extent possible, you want to ensure that the senior is deeply involved in all matters affecting their care and that expectations around changes in their regimen are clearly spelled out. They are the central part of the care team and should have a say in important decisions around their own treatment.
You, the caregiver. You’re the senior’s #1 advocate and are charged with orchestrating a slew of appointments, specialists, and medical information, as well as follow-up appointments. Your primary goal is to ensure the senior is understood before these providers and that you both have the necessary information to make critical care and treatment decisions and implement the doctor’s orders.
Primary Care Provider (PCP), or Primary Care Physician, is often the doctor (or sometimes, nurse practitioner) that is meant to have the big picture in mind and a clear handle on the patient’s care plan. The PCP is managing the patient’s overall care, which can include addressing other health conditions (chronic and acute), such as arthritis, ear infections, and more.
Endocrinologist. The ‘Endo’ is the patient’s diabetes doctor whose job is to oversee the patient’s overall diabetes care management. They’ll check their A1c at every visit and prescribe and monitor their diabetes medication, insulin, and other approved devices, such as insulin pumps or CGMs. They routinely evaluate a patient’s weight, symptoms, and other vitals.
Nephrologist. A specialist trained in the health of your kidneys. This is the doctor that will drive any dialysis treatment for the senior in your care, as well as any dietary changes. This is certainly true if the senior has been diagnosed with renal failure or renal disease.
Neurologist. A specialist trained in matters related to the nervous system. A patient dealing with neuropathy, where they feel numbness in their legs or hands, may be referred to a neurologist for an additional work-up.
Eye doctor. Individuals with diabetes may be more prone to glaucoma and cataracts. Hence, scheduling regular diabetic eye exams is an important part of the care plan for a person with diabetes. These exams go beyond routine eye exams and check the retina and blood vessels for signs of retinopathy.
Other specialists. You may need to deal with other specialists depending on the other health conditions the senior may be experiencing at any point in time.
Keeping Inventory of Diabetes Supplies

Seasoned caregivers to persons with diabetes are exceptional at keeping an inventory of their stock of diabetes supplies. Keeping a spreadsheet with key information can help you better track everything without finding yourself low on supplies or medication. Our recently developed diabetes tracking sheet can make the process much easier.
Whether you choose a spreadsheet or a handy notebook, document the following:
- Pharmacy name, phone #, and location
- Diabetes supply company name, phone #, and location
- Manufacturing company name, phone #, and location
- Prescription name
- Prescription #
- Dosage
- Name of Doctor prescribing (and their name, phone #, location)
- Total # of refills left
- Amount of supplies remaining (ex. test strips, etc.) and your estimated ‘run out’ date.
- Expiration dates – you never want to use expired Glucagon pen or test strips, for example.
You’ll need to brush up on your math skills. Be sure to count days on the calendar, not months. A 90-day supply of anything will be 90 days, not 3 months from today’s date.
Being off by even a few days in your calculations can leave you without supplies when they’re needed the most. Do your best to calculate the actual usage of supplies and project out, giving yourself some wiggle room (to the extent covered by the insurance company, or that your budget permits).
Adjust the Prescription
If you find that you need more supplies during a given prescription period, talk with your doctor about updating the prescription.
For example, the Tandem infusion sets are supposed to last 3 days. However, we have calculated that my daughter goes through them on an average of every 1.5 to 2 days. We were always short until the doctor updated the prescription.
You can always contact the manufacturer to replace items that are faulty or are not functioning to their standard. We also accidentally dropped 30 test strips into a bucket of water by accident. Unfortunately, there’s no replacing that. At one point, we used to go through 15-25 test strips on a given day, but since she got her insulin pump, we now use a max of 3 to 4. We updated the prescription, so that it isn’t refilled at the same rate and keep the extras that we have as a backup.
Coverage and Restrictions
You’ll want to familiarize yourself with the senior’s health care coverage and any special restrictions. Are they on basic Medicare? Do they primarily rely on their local Community Health Center? Aside from understanding what exams and treatments are covered, you’ll want to be clear on what diabetes supplies are covered.
For example, Medicare Part B and most private health plans cover CGM’s. However, Medicaid coverage of CGM’s varies widely by state. And most insurance companies will only approve insulin pumps after 6 months of diagnosis, or when a provider can make a case for a medical exception (not easy to do).
Replenish in Time
It’s important to replenish supplies in a timely manner to avoid getting stuck without essentials like test strips or needles, or even batteries for a glucometer.
Depending on your health insurance and location, you may be ordering from a local supplier or directly from the manufacturer. Other times, the supplies need to be refilled at your local pharmacy.
Enrolling in mail-order has its pros/cons – convenience, less costly, but a headache to update. And it gets tricky when you have multiple companies to work with.
Finding Free and Low Cost Medication and Supplies
Medication, treatment, and caregiving services for diabetes are expensive. According to the cost estimation by the American Diabetes Association (ADA), the average yearly healthcare expense for patients with diabetes in 2017 was $16,752. This exceeds double the cost of healthcare costs for an individual without diabetes.
Thankfully, there are some approaches that can make supplies easier to afford.
- Patient Assistance Programs (PAP). The PAP is designed to offer FREE diabetes meds. PAPs are managed by drug manufacturers and based on income eligibility, though there is some variation between the companies. You’ll need to visit the manufacturer’s website directly to learn more about their application process.
- The National Council on Aging (NCOA) manages BenefitsCheckup where you can look to see if you or your loved one qualifies for free or low-cost prescription drugs or other resources.
- Walmart. You heard right. Walmart sells just about everything. That now includes low cost insulin, which they began selling in July 2021. The same type of insulin is expected to be sold at Costco / Sam’s Club soon.
- Non-profit agencies can also provide free or low-cost medication, insulin, and diabetes supplies, or a repository of places that do:
- Medicine Assistance Tool has compiled a wealth of information on how to get free diabetes prescription drugs.
- NeedyMeds connects people with programs they may qualify for to access free or low cost medications and related healthcare expenses.
- Rx Hope assists patients and caregivers with the patient assistance program application process and with tracking requests.
- Rx Assist is a directory of patient assistance programs.
- Online Forums. This is your last course of action. You can also look online for diabetes forums, including groups on Reddit, where people offer free supplies to help others in need.
Dialysis

As the caregiver, you may find yourself heavily involved in transporting the senior to their routine dialysis visits. According to the National Kidney Foundation, about 30% of patients with type 1 diabetes and 10 to 40% of patients with type 2 diabetes will eventually suffer from kidney failure.
The severity of kidney disease and the patient’s overall prognosis will determine their options for treatment and type of dialysis. The patient may be placed on a waitlist for a kidney transplant or be referred for ongoing dialysis. Dialysis can be overwhelming for patients and caregivers. It is incredibly time consuming. Getting accustomed to the routine can take some time.
The 3 forms are hemodialysis, peritoneal dialysis, and continuous renal replacement therapy (CRRT). All types come with risks and side effects that you as the caregiver will need to be vigilant in spotting. All have a similar goal – to filter your blood, remove waste, and in essence, replace your kidneys.
- Hemodialysis is the most common type of dialysis and occurs at a hospital, medical office, or dialysis center. An entry point into your veins must be surgically made.
- Peritoneal dialysis can be done at home after a catheter is surgically placed in the abdomen. There are various subtypes and may be an option if the provider feels that the patient can manage.
- CRRT is only done in the hospital to treat acute cases of kidney failure, almost around the clock.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the National Kidney Foundation offer excellent resources to help caregivers to understand what to expect about the various treatment options and their side effects.
Conclusion
Type 1 and type 2 diabetes are complex diseases, requiring people to pay attention to many things, including their blood sugar levels, their diet, symptoms that might indicate a significant problem, medications, doctor’s visits, and more. Outcomes are also influenced by people’s ability and willingness to follow the course of treatment set to them.
However, medication and healthy lifestyle practices, combined with routine home care can help elderly diabetic people live a good and healthy life, free from serious complications.
Caregivers often play a vital role in this process, making it easier for seniors to understand what’s needed and helping them with diabetes care tasks that the senior can’t manage alone. Even simply the emotional support you provide can make a huge difference to a diabetic senior.

Leave a Reply